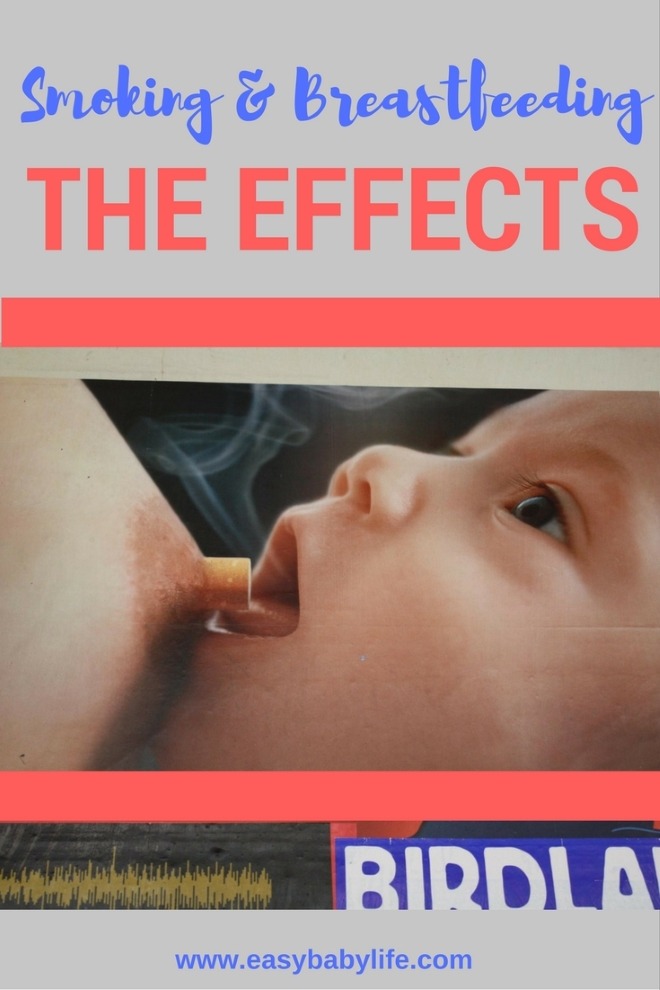
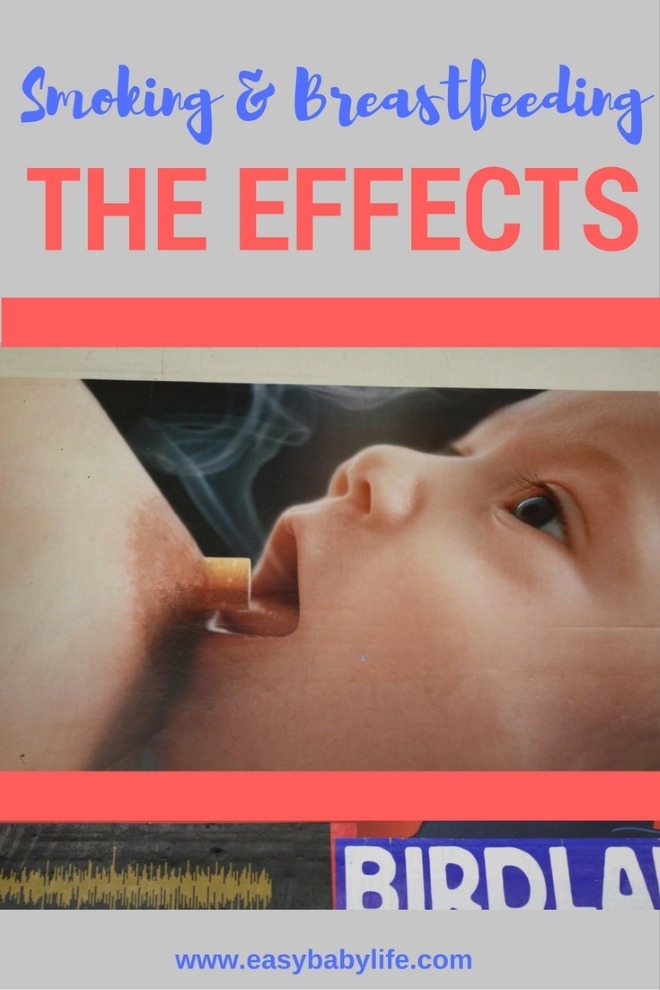
Is smoking while breastfeeding safe? What are the effects of smoking while breastfeeding?
Let’s take a look at the effects on your baby of smoking when you breastfeed, and how you can handle the situation in the best possible way for your child.
When a mother is smoking while breastfeeding, it comes with a risk. This risk is primarily because of nicotine in cigarettes, and we all know that this substance is very bad for any human being, much more for a baby whose body is still developing quickly. But there are other problems as well.
What are the effects of smoking while breastfeeding? Who decides if you should stop or not? Why not learn more about the effects of smoking while breastfeeding first, then make your decision after?
8 Effects of Smoking While Breastfeeding
- Changes the Taste of the Breast Milk
- Early Weaning
- Smoking Inhibits the Milk Production
- Increased Risk of Respiratory Illness
- Irritability, and Colic
- Diarrhea, Vomiting, Faster Heart Rate, Nausea
- Sleep Disturbances
- Secondhand Smoke and SIDS
- Smoking and Breastfeeding or Formula-feeding
- Rules of Thumb to Reduce the Risks for Your Baby
Changes the Taste of the Breast Milk
When nursing a baby, it must be emphasized that what you eat and drink will affect the milk you feed your baby. This includes the nicotine you ingest when smoking.
High levels of tobacco chemicals get transferred into breastmilk. Therefore, if you smoke while breastfeeding, your baby is likely to get exposed to nicotine early in life. The amount of nicotine to which the baby is exposed depends on several variables, such as the number of cigarettes that the mother smokes per day and the time interval between the last cigarette and the beginning of breastfeeding.
The nicotine alters the taste of your milk, which your baby may not like. This may reduce their willingness to eat or lead to earlier weaning.
Some studies suggest that smoking reduces the amount of fat in breast milk, which also negatively affects the taste and the baby’s willingness to breastfeed. For example, it has been shown that the milk of smoking mothers has about 23% lower lipid content than the milk of non-smoking mothers.
However, there are ways to avoid exposing your baby to nicotine by smoking after breastfeeding instead of before and not smoking at least 2 hours before feeding.
Early Weaning
Statistics show that babies exposed to nicotine tend to be weaned earlier than babies who were not exposed to nicotine. There are different theories about why this may be the case.
For example, one explanation is that the baby might refuse the milk because of the taste or insufficient milk supply.
Another suggestion is that the mother might not be as interested in breastfeeding her child because of the conflict between smoking and nursing. Some mothers may decide to stop breastfeeding earlier because they fear the toxic effect nicotine and other substances that are transferred to breast milk may have on their babies.
One study showed that those mothers who smoked more than 10 cigarettes daily postpartum were 2.3-2.4 times more likely than non-smokers to not breastfeed after 10 weeks.
Furthermore, it was shown that when the mother smokes more than 5 cigarettes a day, their breastfed babies show behaviors that may also promote early weaning, such as colic or crying.
Smoking Inhibits the Milk Production
Smoking may lower the amount of breast milk produced. This is because prolactin, a protein hormone responsible for stimulating milk production, decreases by as much as 50% when smoking. This causes lower milk volume and a lower fat concentration in the milk.
Some studies showed that when a mother smokes more than 10 cigarettes a day, her milk supply decreases, and the milk composition alters.
Increased Risk of Respiratory Illness
Smoking directly affects the health of your lungs, and by breastfeeding your baby, you expose them to possible respiratory illnesses. At such a young age, the baby will have destructive nicotine in the respiratory system, and if their genes and general physical health are not strong enough to fight respiratory ailments, they may have to deal with a life-long problem of respiratory illness.
Although it is established that breastfeeding protects against respiratory tract infections, this reduction of risk may be lost when the mother is smoking.
Irritability and Colic
Anyone who has been near a baby with colic knows how hard it is on both baby and parent with the long crying spells and disturbed sleep patterns.
Some studies suggest that the mother’s smoking during breastfeeding increases the baby’s risk of colic. The more the mother smokes, the higher the chances that the baby will suffer from colic. This higher risk of colic is established already during pregnancy if the mom smokes.
The results of another study, however, did not show a significant association between smoking during breastfeeding and colic. Instead, it was confirmed that smoking during pregnancy is indeed associated with an increased risk of colic.
These results suggest that if the mother didn’t smoke during pregnancy but smokes during breastfeeding, the baby’s risk of colic will be the same as for the babies of non-smoking breastfeeding mothers. Therefore, it seems that exclusive breastfeeding might be protective against colic, even if the mother is a smoker.
As you can see, the research is inconclusive regarding the link between smoking while breastfeeding and colic, but there may be an increased risk, and especially if you smoked during the pregnancy too.
Sleep Disturbances
Even if your baby doesn’t get colic, one study has shown that babies sleep significantly less (almost 40% less) during the hours after their mother smoked and they breastfed, compared to days when their moms abstained from smoking.
According to one study, babies who were breastfed immediately after the mother smoked slept 53.4 minutes on average, compared to 84.5 minutes in babies whose mothers didn’t smoke before breastfeeding. Another good reason for any sleep-deprived mom to let go of the cigarettes!
Diarrhea, Vomiting, Faster Heart Rate, Nausea
Diarrhea, vomiting, increased heart rate, and nausea are other unpleasant symptoms that babies exposed to cigarette smoke and nicotine sometimes suffer from.
Secondhand Smoke and SIDS
It has been proven that secondhand smoke, in general, is even more toxic than the smoke inhaled by the smoker.
For example, secondhand smoke causes even higher incidents of ear infections among babies.
Secondhand smoke also increases the risk of SIDS (Sudden Infant Death Syndrome). The number of SIDS cases has been significantly decreased with interventions such as “Back to Sleep,” which emphasize the importance of placing the baby on their back for all sleep times.
However, it was shown that some infants who die of SIDS have a higher concentration of nicotine in their lungs, as well as cotinine, than infants who die of other causes.
This being the case, it is very important that if you plan to continue smoking while breastfeeding, the very least you should try to do is to stay away from your baby when you smoke and avoid smoking inside your home or your car because the smoke can linger.
Smoking and Breastfeeding or Formula-feeding
In conclusion, the disadvantages of smoking while breastfeeding are tremendous; the cards are stacked up against the
child.
So, does that mean that you should stop breastfeeding if you can’t stop smoking?
Actually, not at all!
Medical experts and doctors would rather have a smoking mother who breastfeeds than a smoking mother who gives formula milk. This is because of the nutritious value of breast milk that can more than compensate for the ill effects of smoking on the baby’s health, at least when compared to those babies who are formula-fed and their mother is a smoker.
For example, it was shown that breastfeeding had still promoted growth and protected babies from infections, even when they were exposed to tobacco smoke. Breastfeeding was also shown to counteract the effect of passive smoke on lung function and the growing respiratory organs.
Thus, even though smoking while breastfeeding is fraught with potential problems, it is not discouraged that much. Ideally, you should quit smoking – forever. But, unfortunately, this is something easier said than done. Just be aware that you will potentially be facing serious health issues – both you and your child, and these are situations that cannot always be reversed.
But, if you simply can’t or won’t stop smoking, then try to extend the time you breastfeed for as long as possible!
Rules of Thumb to Reduce the Risks if Smoking When You Have a Baby
To conclude, here are some rules of thumb to reduce the health risks for your baby if you continue to smoke:
- Never smoke close to your child or in the same house or car, since secondhand smoke is very dangerous
- Limit the number of cigarettes to well below 10 per day
- Smoke after breastfeeding instead of before and avoid smoking at least 2 hours before breastfeeding
- Continue to breastfeed for as long as possible
- Do NOT stop breastfeeding to protect your child or to make life more convenient; breast milk is better than formula if you smoke
Read Next About Breastfeeding
- How the Breastmilk Taste Depends on Mom’s Diet and Why to Care
- 18 Awesome Breastfeeding Benefits For Baby And Mom
- 9 Magic Components Of Breast Milk and How They Benefit Your Baby
Research References
Ahmed, F., Jean-Baptiste, F., Thompson, A., Nwokorie, U., Nya, G. E. & Bassey, G. O. (2019). Effects of maternal tobacco smoking on breast milk composition and infant development: a literature review. Journal of Bacteriology & Mycology, 7(5), 107-110. DOI: 10.15406/jbmoa.2019.07.00254
Amir L.H. & Donath S.M. (2002). Does maternal smoking have a negative physiological effect on breastfeeding? The epidemiological evidence. Birth, 29(2), 112-123. DOI: 10.1046/j.1523-536x.2002.00152.x
Canivet C.A., Ostergren P.O., Jakobsson I.L., Dejin-Karlsson E. & Hagander B.M. (2008). Infantile colic, maternal smoking and infant feeding at 5 weeks of age. Scandinavian Journal of Public Health, 36(3), 284-291. https://doi.org/10.1177/1403494807086981
Dorea J.G. (2007). Maternal smoking and infant feeding: breastfeeding is better and safer. Maternal and Child Health Journal, 11(3), 287-291. DOI: 10.1007/s10995-006-0172-1
Kukla L., Hrubã, D. & Tyrlik M. (2008). Trends in respiratory morbidity of children in relation to their passive smoking exposure. Casopis Lekaru Ceskych. 147(4), 215-221.
Liu, J., Rosenberg, K. D. & Sandoval, A. P. (2006). Breastfeeding duration and perinatal cigarette smoking in a population-based cohort. American Journal of Public Health, 96(2), 309-314. doi: 10.2105/AJPH.2004.060798
Mennella J.A., Yourshaw L.M. & Morgan L.K. (2007). Breastfeeding and smoking: short-term effects on infant feeding and sleep. Pediatrics, 120(3), 497-502. doi: 10.1542/peds.2007-0488
Özalp, E. C. & Yalçın, S. S. (2021). Is maternal cigarette or water pipe use associated with stopping breastfeeding? Evidence from the Jordan population and family health surveys 2012 and 2017–18. International Breastfeeding Journal, 16(43). https://doi.org/10.1186/s13006-021-00387-z
Primo, C. C., Ruela, P. B., Brotto, L. D., Garcia, T. R. & Lima, Ede F. (2013). Effects of maternal nicotine on breastfeeding infants. Revista Paulista de Pediatria, 31(3), 392-397. doi: 10.1590/S0103-05822013000300018
Stroud L.R., Paster R.L., Goodwin M.S., Shenassa E., Buka S., Niaura R., Rosenblith J.F. & Lipsitt L.P. (2009). Maternal smoking during pregnancy and neonatal behavior: a large-scale community study. Pediatrics, 123(5), 842-848. doi: 10.1542/peds.2008-2084
U.S. Department of Health and Human Services. (2014). The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. Centers for Disease Control and Prevention. https://www.cdc.gov/tobacco/data_statistics/sgr/50th-anniversary/
Image: Courtesy of Reut C

Paula Dennholt founded Easy Baby Life in 2006 and has been a passionate parenting and pregnancy writer since then. Her parenting approach and writing are based on studies in cognitive-behavioral models and therapy for children and her experience as a mother and stepmother. Life as a parent has convinced her of how crucial it is to put relationships before rules. She strongly believes in positive parenting and a science-based approach.
Paula cooperates with a team of pediatricians who assist in reviewing and writing articles.